Obesity is a growing concern in the UK, affecting over two-thirds of adults in England. While the physical health risks of obesity are well-documented, the impact on mental wellbeing is often overlooked. This intricate relationship between obesity and mental health deserves attention, as they can significantly influence each other.
Obesity and Mental Health
The link between obesity and mental health is complex and operates in two directions. Here’s a closer look:
- Obesity Leading to Mental Health Issues
- Body Image and Self-Esteem: Carrying excess weight can lead to body image dissatisfaction and low self-esteem. This can trigger feelings of shame, anxiety, and social isolation.
- Depression and Anxiety: Research suggests a strong correlation between obesity and depression. People with obesity are at a higher risk of developing depression, and vice versa. The exact reasons remain under investigation, but factors like chronic inflammation and changes in brain chemistry might play a role.
- Discrimination and Stigma: Societal weight bias and discrimination can significantly impact mental health. People with obesity may face prejudice in various aspects of life, leading to feelings of isolation, anger, and frustration.
- Reduced Quality of Life: Obesity can limit physical mobility and participation in activities one enjoys. This restricted lifestyle can contribute to feelings of worthlessness and decreased overall well-being.
2. Mental Health Contributing to Obesity
- Emotional Eating: Some individuals turn to food for comfort or to cope with stress, anxiety, or depression. This can lead to unhealthy eating patterns and weight gain.
- Medications: Certain medications used to treat mental health conditions can have weight gain as a side effect, further complicating the issue.
- Reduced Motivation: Mental health issues like depression can lead to decreased motivation for physical activity, which can contribute to weight gain.
It’s important to remember that the relationship between obesity and mental health is not always linear. Several factors, including genetics, socioeconomic status, and access to healthcare, can influence how they interact in each individual.
Seeking Help and Support
If you’re struggling with obesity and its impact on your mental health, here are some steps you can take:
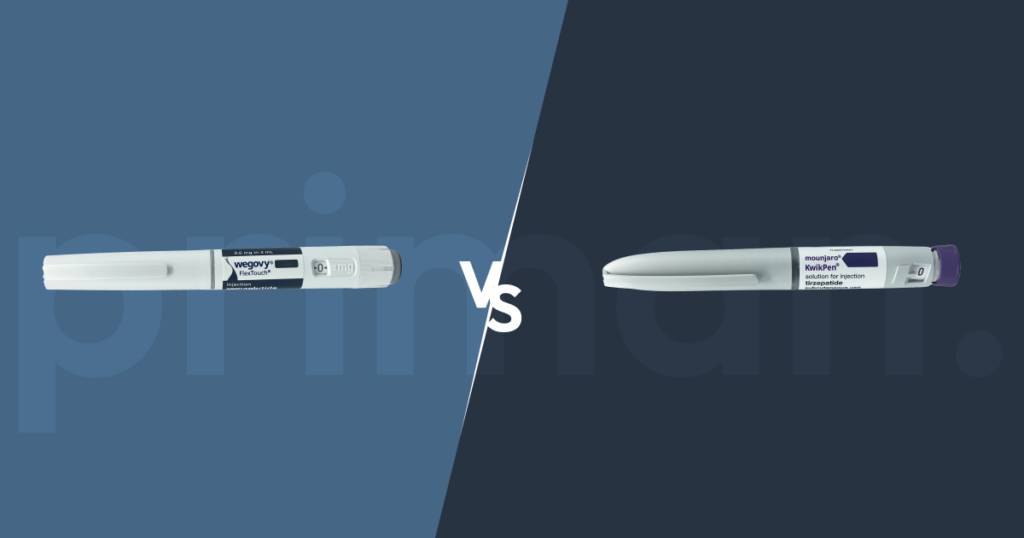
- Talk to Your Healthcare professional: Your clinician can assess your situation, provide support, and connect you with appropriate services, such as weight management programs (weight loss medications such as GLP 1 injections (Wegovy, Mounjaro etc..) or mental health professionals.
- Consider Therapy: Cognitive behavioural therapy (CBT) can be an effective tool to address negative body image, develop healthy coping mechanisms, and improve overall well-being .
- Seek Counselling: Talking to a counsellor can help you develop healthy coping mechanisms for stress and emotional eating, and address any underlying mental health issues.
- Join a Support Group: Connecting with others who understand the challenges of weight management and mental health can be incredibly helpful.
- Prioritise Self-Compassion: Accepting yourself as you are while working towards a healthier lifestyle is crucial. Focus on progress, not perfection.
- Focus on Healthy Habits: Make small, sustainable changes to your diet and exercise routine. Celebrate non-scale victories like increased energy or improved mood.
For healthcare professionals – It’s important to screen for both obesity and mental health issues during patient consultations. A holistic approach that addresses both physical and mental health needs is crucial for successful weight management and improved overall well-being.
Key Takeaway
Obesity and mental health are intricately linked. Understanding this connection is key to addressing both effectively. By prioritising self-care, seeking professional support, and adopting healthy habits, individuals can break free from this two-way street and achieve better physical and mental health.
References
Blasco, B. V. et al. (2020) “Obesity and depression: Its prevalence and influence as a prognostic factor: A systematic review,” Psychiatry investigation, 17(8), pp. 715–724. doi: 10.30773/pi.2020.0099.
Overweight and obesity in adults (2022) NHS England Digital. Available at: https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-for-england/2021/overweight-and-obesity-in-adults
Psychological perspectives on obesity (2019) BPS. The British Psychological Society. Available at: https://www.bps.org.uk/psychologist/psychological-perspectives-obesity
Puhl, R. M. and Heuer, C. A. (2010) “Obesity stigma: Important considerations for public health,” American journal of public health, 100(6), pp. 1019–1028. doi: 10.2105/ajph.2009.159491.